Balls and Walnuts
more than you ever wanted to know
- About
- All Change
- Big pix
- Dormies
- Ear, Nose, Throat, and Soul
- Heaven on Earth
- Karen’s memoriam . . . booklet and eulogy
- Lyvvie’s email
- Magic Schoolbus does your nose and throat
- Nest: scene one
- Sex and the Single Wendigo
- Sprouts
- The Mechanic
- Two Birds, One Stone
- Excerpt: Gator and Shark Save the World
Category Archives: The Barbarous Craft
CME
Why is it that I complain about the heat constantly, but love to have the shower as hot as I can stand it?
Perhaps “a dry heat” isn’t all it’s cracked up to be.
We had a Continuing Medical Education activity tonight, a lecture on Valley Fever. Here in Kern County, we have the distinction of being a Valley Fever hot spot. It’s endemic throughout the Southwest, but here it’s big. We are the Valley in Valley Fever, after all.
What I learned tonight:
There’s no vaccine. Not even a glimmer of one on the horizon.
If you get it in your meninges (the tissue enclosing the brain), you’ve got it for life, and you’re in for a lifetime of treatment. But at least there is treatment. In the old days, most of these folks would die in the first year.
You can’t get it by working outside in your garden. Treated soil — soil that’s been watered, fertilized, etc. — does not harbor the fungus. So you’d think you’re safe as long as you don’t hang out in construction sites or go dirt-biking in the wilderness, right? Wrong. This shit can travel, wind-borne, for 35 miles or more.
You’re better off with a bad case of tuberculosis than with a bad case of Valley Fever.
As bad as the situation is with antimicrobials, what with the constant emergence of resistant organisms, the situation with antifungals is far worse. Our main fungicidal (fungus-killing) is Amphotericin B, a drug that punches holes in fungal cell membranes, allowing leakage of electrolytes and eventual death of the fungal cell. Unfortunately, it does the same thing to animal cells, hence the high toxicity of Amphotericin (AKA amphoterrible). Other anti-fungals are fungistatic, meaning they halt growth but don’t kill the organism.
Well, that’s all I can think of right now. I’m sure I learned more 🙂
D.
Hands-off medicine

Bend over, I need to check your doody.
My Sis was bemoaning the fact that all her new internist did was listen to her heart, look in her ears, and check her throat. Frankly, I’m surprised she did that much. My last three docs (always changing docs because we’re always MOVING, go figure) reviewed my meds, checked my BP, and asked what drugs I needed refilled. End of story. Do you think my wife, who actually has some trouble, gets a closer look? Not really. They like to tap out her reflexes.
Notwithstanding the countless texts written in the 19th and 20th centuries predicated on the value of physical diagnosis (Zachary Cope’s Early Diagnosis of the Acute Abdomen comes to mind, for one), one could make an argument that an internist’s job nowadays breaks down to algorithms crunching raw data: patient’s age? sex? family history? smoker y/n? drinker y/n? list of medications? and so forth. Turned fifty, let me send you for a colonoscopy. Eighteen months since your last mammogram, ooh, you’re overdue for another. Same goes for that pap smear. Not taking baby aspirin, well, take a baby aspirin.
I’m not an internist. I’m a surgeon. I practice physical examination and physical diagnosis with each and every patient I see. I’d be lost without my hands and eyes. Since I’m not an internist, you could argue I have no business criticizing them. And I don’t, and I’m not. What I want is to draw attention to the perception that internists are data crunchers who no longer practice the laying on of hands.
If we notice it, others will, too. Health care administrators, health insurance executives, health care policy wonks and politicians will notice. And what happens when these folks decide that the internist’s job can be replaced by a fairly unsophisticated computer program?
I do think that internists, most of them, bring a lot more to the exam table than would a computer program. I suspect they could argue very well for the necessity of their existence. But one thing I’ve learned in medicine these past 25 years: we doctors have little control over our own destinies. Bureaucrats have done a tidy job altering our professional lives to suit their fancies.
So doesn’t it seem logical that internists should strive to win the perception war before someone without an MD or DO after his name tries to debate them out of existence?
D.
Some things never change
Still reading Charles Bukowsky’s sort-of-memoir Ham on Rye, and I was struck by his description of clinic at LA County Hospital, circa 1936. The patients all had a little slip of paper stating their appointment time: 8:30 AM. If you didn’t check in at 8:30, you were out of luck. You would come in and you would sit. And sit. And sit. If you left and they happened to call your name, you were out of luck. If something came up and the docs were seeing an ER patient and couldn’t come to clinic, you were out of luck. And God help you if you had something interesting — then they’d bring all the other residents and med students by to gawk at you, and they’d talk about you like you were a side of beef.
During my time at LAC, it was much the same. Yeah, even though 60 years had passed . . . And I can’t say that we were any more empathetic than our 1930s counterparts. We did the same thing. Once, when I was a med student on my dermatology rotation, I saw a teenage boy with pearly penile papules (warning — photos!) I told him that I didn’t know what this was, and I would have to bring in my attending to look and tell us both what he had. He clammed up. It was difficult enough showing ONE guy his dick — now he’d have to show two?
My attending came in, exclaimed, “BY JOVE! It’s pearly penile papulosis!” (He may not have said “By Jove”) and disappeared from the room. The boy and I were mystified. And then, to both our horror (his more than mine), the attending returned trailing three med students, two of whom were female.
Great teaching case.
And if that didn’t thrill ya, I bring you a little video I like to call, “Fv(K with me, will ya?”
D.
An anniversary of sorts
I had my first patient today who was seeing me for his one year followup. I can’t remember when I started with the new job — second week of July, 2009, I think. (Ah, here we go.) So I passed the “real” anniversary some time ago.
But in a way, this is the only anniversary that counts.
One of the rewards of being in private practice in the same community for ten years was the joy of watching some people grow up . . . and some grow old. I miss that. It will be a while before I get that feeling of connectedness here in Bako, but somehow passing my Year One anniversary makes me feel a little closer to that goal. Now if only someone would cure this aging thing, because life is going by way too fast.
Do you realize if medical research comes up with true life extending technologies, that will be the end of retirement? Or at least, the end of State-funded or corporate-funded retirement. Self-funded retirement could still work. But you have to ask yourself just how long you could tolerate a life of leisure. I suspect most folks would go back to work (or stay at work).
I wonder: if we had complete control over our work week, and we were working solely for the pleasure of it and not to earn money, how many hours would we work per week, on average?
D.
Trouble either way
From the first clinical rotation in med school, we’re taught, Do the right thing. It’s an obvious lesson, but it’s the sort of thing which bears endless repetition, since human nature seems bent in the opposite direction. See the ER consult now, or sleep a bit more until they page you again? Check those stat labs, or go home five minutes sooner? After a while it becomes reflexive; you do the right thing without even listening to what your body wants to do.
Those are the easy decisions.
But then there are the questions that have no right or wrong answer. Operate now when the patient is unstable, and the risks necessarily higher? Or wait until the patient is stable, but take the chance he could get worse during the time it takes to stabilize him? It’s one of those decisions that could trip you up no matter which way you fall. You need a crystal ball or a reliably prescient gut for questions like this. And no one’s gut is that prescient.
Reminds me of the painting I had up in my private practice office: carnival fortune teller, dead eyes suggesting she’s an automaton, catering to three twins, each of which has fingers crossed behind his back. People would ask what it meant. I’d say, “I don’t have a crystal ball.”
Ultimately, I tend to use the same thought process I do whenever a parent says, “You’re only taking the adenoids out? Why not take the tonsils, too, while you’re at it?” This only comes up if I have already decided the tonsils aren’t causing problems. In essence, the parent is asking me to take out the tonsils to prevent a future problem. Same way a general surgeon doing an exploratory laparotomy will usually take out an appendix whether it’s hot or not.
My thinking: why incur additional risk now for something that might become necessary in the future? In twenty years, I’ve only been wrong once. So we had to put someone to sleep two times when one time might have served. Balance that against all the unnecessary operations I would have done, had I been more aggressive.
But the stakes are low in that scenario. Much tougher to know what to do when someone’s life is on the line and will continue to be on the line whether I opt for path A or path B. It could go either way, and the only way to know, truly, the right thing to do, is to have access to that damned crystal ball.
D.
Wherein I get told by a five-year-old
My patient is wearing this cute white-and-blue thing, kind of tie-dyed with raggedy frills sewn on here and there, Flash Dance meets the 60s hippie chic. She’s terribly cute.
“What a pretty dress!” I told her. “I’ve never seen anything like it.” Which was true.
“Thank you,” she said. Then, “But it’s not a dress. It’s a skirt plus a top.”
I frowned at her, as ogre-like as I could make myself. “What do I know? I’m a guy.”
And then her mom and I cracked up and I couldn’t get any more work done for the next couple minutes.
D.
Well, duh.
I’m wonderful. My patient just told me so. “You’re wonderful,” she said, and in case I hadn’t heard, she repeated it twice, and when I asked her to repeat this to my medical assistant, she did so. Happily.
“He’s wonderful,” she said.
“I know,” said my assistant.
Which raises the question, why doesn’t my wife ever say this to me? Have I not given her ample evidence of my wonderfulness?
Maybe Karen would tell me I’m wonderful if I cleaned the wax from her ears, too.
D.
Working on becoming the world’s youngest laryngectomy patient?
Toddler down to 15 cigarettes per day.
That links to a video of a rather chunky three-year-old (by my guess) puffing like a veteran. As docs, we regularly take a smoking history from our patients. Do you use tobacco? Smoke, chew . . . which? How much? When did you start?
This all translates into a metric, the “pack-years” logged by the patient. The earlier you start and the more you smoke, the higher your pack-years. All of us remember our record-holder. Mine was 120. How does a sixty-something guy log 120 pack-years? By starting at age five and averaging two to three packs per day.
How does this happen? Uncles, grandparents, sometimes even parents give the kid a cigarette — you know, because it’s cute. And we’re talking about nicotine, one of the most (if not THE most) addictive substance known to humankind, more addictive than heroin or cocaine. Doesn’t make much work to turn the kid into a coffin nail junkie.
These kids, they’d probably be doing themselves less damage swigging 40-ounce bottles of malt liquor. And they’d look much cuter doing it, too.
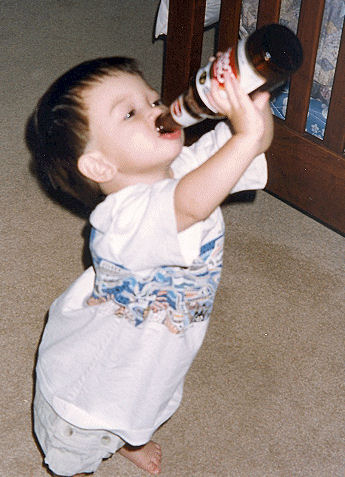
The things we do to our kids . . .
D.
This must be some kind of mitzvah. How do you say cockroach in Hebrew?
I got my patient in ASAP. You’d want to get in ASAP too if you had something crawling in your ear. I expected to find the usual cockroach, and indeed, my patient did not disappoint. But it was more than a cockroach.
It was Cockroach Plus.

Uh oh theca.
Cockroach plus ootheca, to be exact — an egg case. This was a female caught embarazada. Knocked up. Up the duff. On stork watch. Wearing the apron high. In the pudding club. Eating for 48.
And she was desperately trying to fulfill her Darwinian destiny in her last moments on Earth.
By the way, the egg case pictured above belongs to a Madagascar hissing cockroach, a beastie we used to breed in days of yore. And if you had one of them in your ears, you’d really have something to worry about.
Don’t know why Cockroach Plus should be so much more disturbing than Just Plain Roach, but it was. But hey, I’m a professional. I squirted some lidocaine down the ear canal (paralyzing and more or less killing the critter) and removed it piecemeal with suction and alligator forceps. End result, one happy patient who took the roach-bits home wrapped in gauze. So who knows, perhaps that egg case will find a happy home after all.
I told Karen all about it. She wanted to know, why didn’t it just back out?
“They can’t back out. Didn’t you know that? Don’t you remember the earwig episode on Night Gallery? They have to eat their way through to the other side.”
“Oh. Night Gallery. That’s your authority on this, huh?”
Yup, that’s my story, and I’m sticking to it. If it weren’t for me, the she-roach would have eaten it’s way through, laying eggs en route to the other side. Hey! I just remembered, there is a phrase for this in Hebrew — pikuach nefesh.
To save a life.
D.
You Don’t Know Jack
Believe it or not, in med school we did receive instruction in medical ethics. Our teacher was a minister, if I remember correctly, but he usually did not have much of a judaeochristian bias — at least, none that I could detect at the time. One day, he talked to us about euthanasia, and while sympathetic to the cause of euthanasia’s proponents, he felt certain that doctors had no business practicing euthanasia. “We need another professional specialty altogether,” he said. “Call them thanatologists.”
The two things I remember from that moment: the uncannily bright grin of one of my classmates, a fellow we’d nicknamed Mickie Mouse for his uncannily bright grins, and who would eventually go into psychiatry; it was as if the clouds had parted and he had looked upon the face of God. Like he had found his home. Sometimes I wonder what he’s up to*.
The other thing I recall: a loud and persistent thought. Why isn’t this our domain? It’s all a matter of how you view doctors. If our role is to keep people alive, then yes, euthanasia is a clear conflict of interest. But if our role is to relieve pain and suffering, then euthanasia should be part of the job.
About this time, the late 1980s, Jack Kevorkian was just getting started in his role as “death counselor,” soon to be death facilitator, eventually to be known to the media as Dr. Death. The media loved to portray the man as a ghoul. Sometimes I suspect that he reveled in this caricature; his artwork, which could best be described as “fitting for the Night Gallery,” would do nothing to destroy this image.
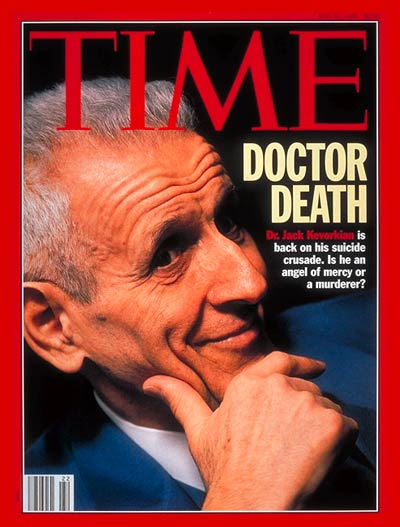
Knowing Time Magazine, I wouldn't be surprised if they had picked murderer.
While Kevorkian initially acted as a facilitator, he ceaselessly pushed the envelope. As long as he served as facilitator and not prime actor, he was judicially unscathed, thanks to the craft of lawyer Geoffrey Fieger and the sympathies of the juries. (When people are forced to confront the prospect of their own deaths, few would not want the option of a painless passing.) But when he himself administered the euthanasia drug to an ALS patient and then arranged for the videotape to be broadcast on 60 Minutes, the D.A. went after him. Kevorkian unfortunately represented himself in this case, and was ultimately convicted of second degree murder. He was ultimately paroled in 2007 after a little over 8 years in prison.
You Don’t Know Jack (HBO) is a wonderful bit of docudrama, not to be missed. Susan Sarandon stars as Hemlock Society member Janet Good, John Goodman as Kevorkian’s friend and assistant Neal Nicol, and Al Pacino plays Kevorkian himself. And while I like Pacino in just about anything he does, I have to admit that lately, Pacino plays Pacino and it’s rare to see him play anyone else. But in You Don’t Know Jack, Pacino lives and breathes Kevorkian. If you’ve ever watched Kevorkian on TV (and if you haven’t, I’d be surprised if he isn’t well represented on YouTube), you’ll find the resemblance striking. Also remarkable casting: Danny Huston as lawyer Geoffrey Fieger. I had to google “Geoffrey Fieger” to make sure he wasn’t playing himself.
I can’t praise this one enough, people. It’s a thoughtful, albeit biased analysis of the issue of doctor-assisted suicide. If you’re looking for a character in this film who can provide a cogent argument against euthanasia, keep looking**. Much like its subject, the movie has an agenda. But it was entertaining, too — funny, poignant, and above all a showcase of terrific acting.
D.
*Ach, what a disappointment. Just googled the man. He’s a successful molecular biologist at U of Chicago . . . not a thanatologist.
**Really, the only argument that comes close to being persuasive is the possibility for abuse by next of kin; but abuse to the point of death can occur in many and varied ways, from neglect to outright physical harm, and the law is there, ready to punish the offender. Euthanasia, since it is such a public act — it must ultimately pass muster with a coroner, I would think — could be easily regulated to greatly reduce the possibility of such misuse.
Find it
Blogroll
- Beth
- Blue Gal
- Charlene Teglia
- Chris and Dean
- Crystal
- dcr, the one, the only
- Erin O’Brien
- Fanatic Cook
- fiveandfour
- Gabriele
- If I Ran the Zoo
- Indecision 2008!
- jmc
- Kate Rothwell
- Kris Starr
- Lyvvie
- Matt’s recovery blog
- Mike Imlay
- Paperback Writer
- Pat Johanneson
- Raw Dawg Buffalo
- Science Blogs
- Shaina
- Shelbi
- Smart Bitches
- Steve Bunche
- Steven Pirie
- Tam’s blog
- The Amanda Files
Archives
Meta
Categories
Pages
- About
- All Change
- Big pix
- Dormies
- Ear, Nose, Throat, and Soul
- Excerpt: Gator and Shark Save the World
- Heaven on Earth
- Karen’s memoriam . . . booklet and eulogy
- Lyvvie’s email
- Magic Schoolbus does your nose and throat
- Nest: scene one
- Sex and the Single Wendigo
- Sprouts
- The Mechanic
- Two Birds, One Stone